End of life care
Please note that the information on this page is out of date and is scheduled for review
Recognition by healthcare professionals of when a person is nearing the end of their life and then responding appropriately plays an essential role in determining whether or not that person has a ‘good death’. This means the person:
- Being treated as an individual, with dignity and respect;
- Being without pain and other symptoms;
- Being in familiar surroundings; and
- Being in the company of close family and/or friends.[1]
Making this possible requires not only excellent clinical decision-making, but timely care decisions in consultation with the individual and the family.
Evidence suggests most people would prefer to die at home, however currently almost half die in hospital.[2] Ensuring a person is able to die in a place of their choosing often involves multiple agencies working closely together to co-ordinate the support they provide. These agencies can include general practitioners, community nurses, domiciliary and adult social care services, hospital and ambulance services, pharmacies, specialist and allied health professionals, hospices and other voluntary sector organisations. However, research suggests end of life care is inconsistent across the country and a range of indicators.
Although hospital is still the most common place of death, in line with the trend nationally, the proportion of deaths occurring in hospital has deceased over the past decade, from 43.6% in 2012 to 36.2% in 2021.
Figure 1: Deaths in hospital (all ages)
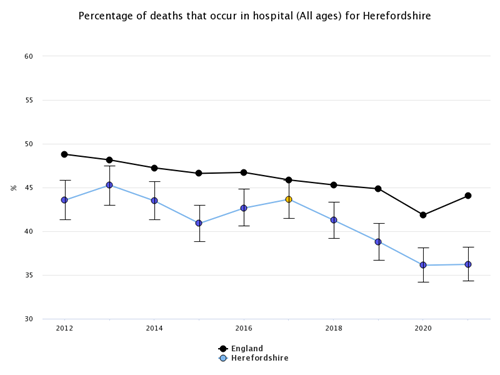
Source: Office for Health Improvement & Disparities, Palliative and End of Life Care Profiles
Broadly, over the past decade the proportion of deaths occurring at home in Herefordshire increased in line with the national trend and only decreased very slightly during the Covid-19 pandemic. In 2012, 22.5% of deaths occurred at home and by 2021 this figure had increased to 28.6%.
Figure 2: Deaths at home (all ages)
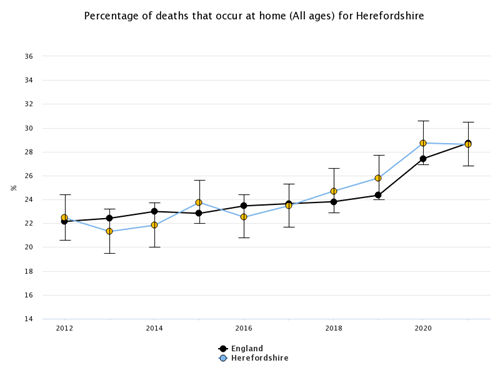
Source: Office for Health Improvement & Disparities, Palliative and End of Life Care Profiles
The proportion of deaths occurring in care homes has increased slightly from 23.5% in 2012 to 25.4% in 2021 - this is significantly higher than in England as a whole (20.2%), likely reflecting the fact that Herefordshire has an older population (which is also ageing more rapidly than nationally).
Dementia presents particular challenges for end of life care because people with dementia may present with signs that suggest they are very close to death, but in fact can show these signs for many months or even years.[4]
For people aged over 65 and diagnosed with dementia, in Herefordshire in 2019, 75.9% of deaths occurred in the deceased’s usual place of residence: a significantly higher proportion than in England (70.3%) and the West Midlands region (66.6%).
In 2019, a significantly lower percentage of people aged 65 and over and diagnosed with dementia died in hospital in Herefordshire than in England or the West Midlands region (24.2% compared to 28.7% and 32.6% respectively).
Figure 3: Deaths in usual place of residence as a percentage of deaths of people aged 65 and over with a recorded mention of dementia:
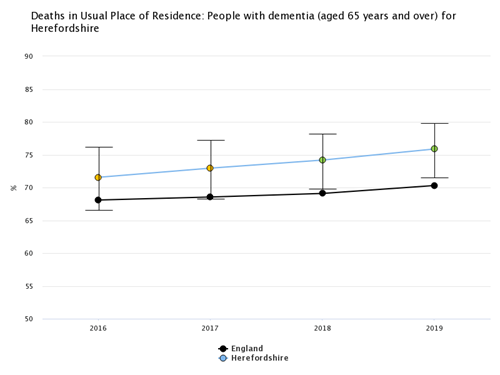
Source: Office for Health Improvement & Disparities, Public Health Profiles.
[1] End of Life Care Strategy: Promoting high quality care for all adults at the end of life, Department of Health, 2008, p.9.
[2] Achieving excellent end of life care locally: How can the public work with Sustainability and Transformation Partnerships to achieve excellent end of life care locally? Hospice UK, 2017. Available at https://www.hospiceuk.org/what-we-offer/publications
[3] End of life care in dementia: An introduction, Social Care Institute for Excellence.